Abstract
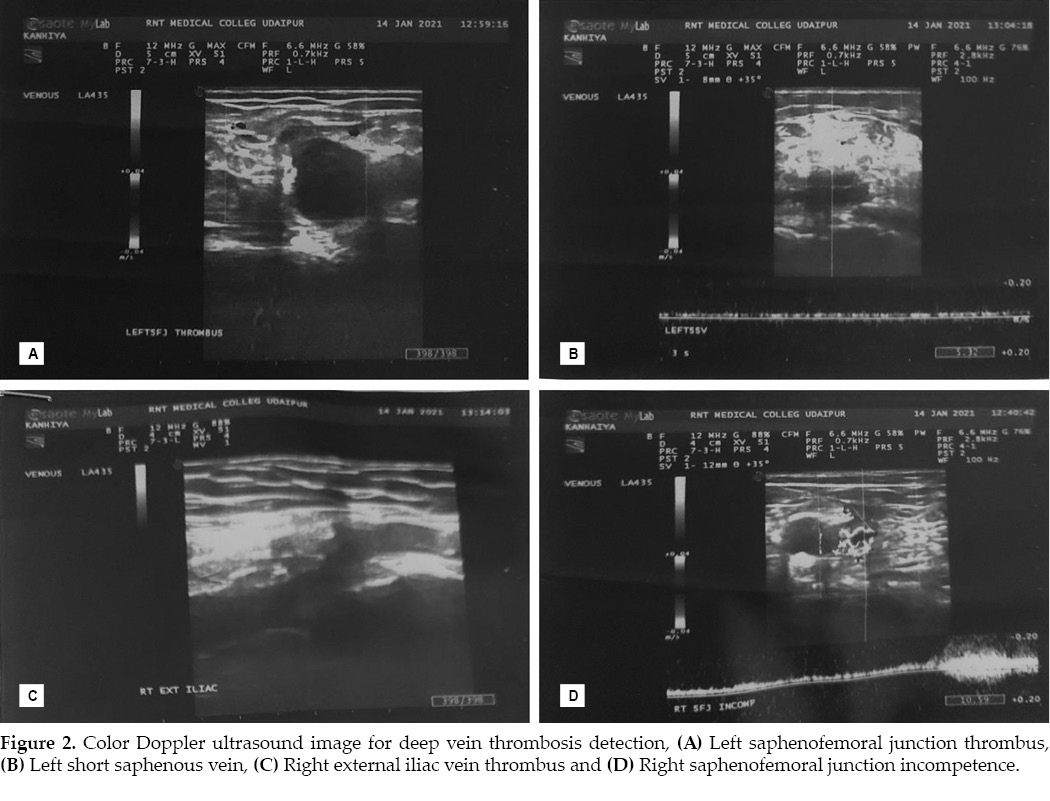
Novel coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become a public health emergency of international concern. In this report, we present a case of a 50-year-old man who presented with mild fever, dry cough and shortness of breath. With suspicion of COVID-19 atypical pneumonia, nasopharyngeal and oropharyngeal swabs were taken and reverse transcription polymerase chain reaction (RT-PCR) was done and found positive. On Day 3rd of admission, he complained of left lower limb swelling, pain, warmth and tenderness which was progressively increasing and also appeared in right lower limb in next 2 days. He had no risk factors for deep vein thrombosis. Bilateral lower limb venous color Doppler ultrasound revealed dilatation and thrombosis in the left external iliac vein, left common femoral vein up to left popliteal vein and its distal branches & left great saphenous vein and in the right external iliac vein, right common femoral vein up to right saphenofemoral junction, with bilateral saphenofemoral junctions incompetence. Anticoagulation therapy was given along with COVID-19 management and patient improved gradually. Currently, there is minimal data available highlighting bilateral deep vein thrombosis in patients infected with COVID-19. This case aims to arouse the healthcare providers for awareness of deep vein thrombosis in COVID-19 case.
Keywords: COVID-19, deep vein thrombosis, pulmonary thromboembolism, SARS-CoV-2
On December 31, 2019, it was informed to the World Health Organization (WHO) that a cluster of cases of pneumonia of unknown cause has been detected in Wuhan City, China. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which caused the pneumonia soon became widespread globally, leading to a pandemic, which has been associated with substantial morbidity and mortality. Novel coronavirus disease 2019 (COVID-19) has spread to more than 200 countries, and the death toll remains very high. Healthcare providers continue to see new and frightening displays of its pathogenicity. Symptoms are similar to the common cold, with most notable symptoms of COVID-19 being fever and dyspnea.1,2 The disease is highly contagious, and the WHO’s weekly epidemiological update on 16 May 2021 reported a total number of confirmed cases 162,184,263 and 3,364,446 confirmed deaths.3 The SARS-CoV-2 enters host cells through the binding of spike glycoprotein to the angiotensin-converting enzyme 2 (ACE2),4 sialic acid receptor, transmembrane protease serine 2 (TMPRSS2) and extracellular slow cell matrix metalloproteinase (CD147). This condition, which causes endothelial dysfunction, is exacerbated by hypoxia and causes thrombosis by increasing blood viscosity as well as the signaling pathway associated with the hypoxia transcription factor. We present here a case involving a 50-year-old male patient with COVID-19 who developed bilateral deep vein thrombosis (DVT).
CASE REPORT
A 50-year-old male admitted to suspected COVID-19 intensive care unit (ICU) in RNT Medical College, Udaipur, Rajasthan with history of mild fever, dry cough and shortness of breath for 5-6 days. He had no comorbidity like diabetes mellitus, hypertension, coronary artery disease, stroke, chronic obstructive lung disease, asthma, hyperlipidemia, cancer or any other history of surgery, trauma, paralysis, paresis or recent cast, bedridden and insect bite in recent past. His vital signs included a temperature of 99°F, pulse rate of 120/min, blood pressure of 100/60 mmHg, respiratory rate of 30/min and oxygen saturation of 60% on room air. Therefore, he was put on noninvasive ventilation.
On physical examination, crepitation was present in both the lung fields, more on left side than right side. No obvious abnormalities were found on the rest of the examination. An electrocardiogram (ECG) showed sinus tachycardia with no acute ST-T segment changes. A chest X-ray posteroanterior view showed multifocal and bilateral ground glass opacities in both lung fields. Laboratory data showed elevated white blood count of 21 × 103/mm3 (with 87.9% granulocytes and 8.1% lymphocytes), hemoglobin of 13.2 g/dL, hematocrit at 40.6% and platelet count of 303 × 103/mm3. The biochemistry reports were within the normal range except for aspartate aminotransferase - 47 U/L (normal range = 15-37 U/L), alkaline phosphatase - 129 U/L (normal range = 46-116 U/L), total protein - 6.0 g/dL (normal range = 6.4-8.2 g/dL), serum albumin - 2.1 g/dL (normal range = 3.4-5.0 g/dL) and also elevated C-reactive protein (CRP) level - 246.77 mg/L (normal range = <5.0 mg/L), lactate dehydrogenase - 962.27 U/L (normal range = <200 U/L), serum ferritin - 373.20 ng/mL (normal range = 22.00-322.00 ng/mL) and D-dimer - 4,983 ng/mL (normal range = <500 ng/mL). His interleukin (IL)-6 level was 4.93 pg/mL (normal value = 0.0-6.4 pg/mL) and prothrombin time-international normalized ratio (PT-INR) value 23 seconds/1.94, respectively. Because of patient presentation, chest X-ray finding and lymphopenia, COVID-19 reverse transcription polymerase chain reaction (RT-PCR) test of nasopharyngeal and oropharyngeal swabs was sent and found positive. The patient received antiviral treatment including remdesivir injection with low molecular weight heparin, steroids, antibiotics and supportive treatment according to the Ministry of Health and Family Welfare (MoHFW) and Indian Council of Medical Research (ICMR) Updated Clinical Management Protocol for COVID-19.5 On day 3rd of admission, he complained of left lower limb swelling, pain, warmth and tenderness which was progressively increasing and also appeared in right lower limb in next 2 days.
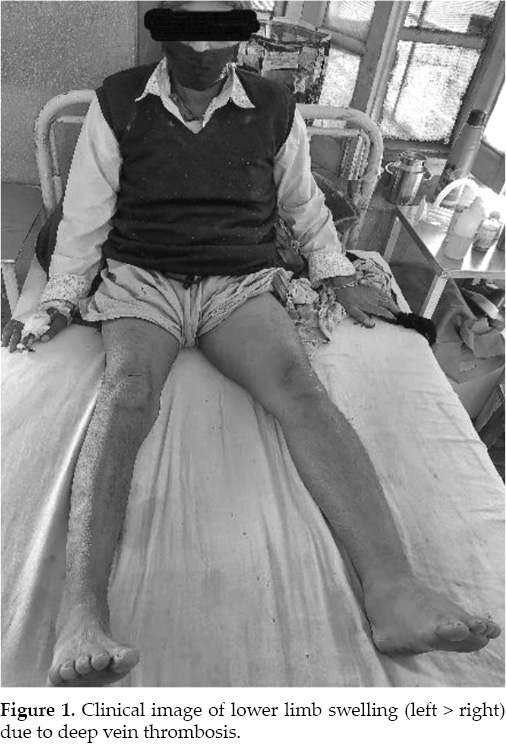
On physical examination, the pain and tenderness were present in both lower limbs and on dorsiflexion of the foot with the leg extended, pain presented in calf of the leg (Homan’s sign positive) (Fig. 1). Bilateral lower limb venous color Doppler ultrasound revealed dilatation and thrombosis in the left external iliac vein and left common femoral vein up to left popliteal vein and its distal branches and left great saphenous vein and dilatation and thrombosis in the right external iliac vein and right common femoral vein up to right saphenofemoral junction and bilateral saphenofemoral junctions incompetence (Fig. 2).
Other tests including antinuclear antibody, anti-double stranded DNA, rheumatoid factor test, anticardiolipin antibodies, factor V Leiden and protein C, protein S tests were normal. Since the patient was hemodynamically stable, tissue plasminogen activator (TPA) administration was not considered. His symptoms significantly improved with anticoagulation. The hypercoagulable panel did not show any other active risk factor for thrombotic conditions. After a week, COVID-19 RT-PCR of nasopharyngeal and oropharyngeal swabs was negative. The swelling and tenderness reduced gradually first in right lower limb and then slowly from left lower limb. The patient was discharged with continuous anticoagulation treatment (warfarin 3 mg daily) and advised to follow-up after 7 days with PT-INR reports (PT-INR value on day of discharge was 23.3 seconds/1.94, respectively).
DISCUSSION
The COVID-19 pandemic started in December 2019 when a cluster of patients presented with pneumonia of unknown etiology that was associated with a seafood market in Wuhan, China.6 The source of this condition was identified as a novel coronavirus, which was later named as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the disease caused by this virus was named as coronavirus disease 2019 (COVID-19). Coronaviruses are enveloped ribonucleic acid (RNA) viruses found among animals such as pigs, bats, camels and cats. As humans acquire these viruses, they commonly result in mild-to-moderate upper respiratory diseases. Three of the coronaviruses are now known to cause severe, and fatal disease in humans, which include severe acute respiratory syndrome (SARS) coronavirus, Middle East respiratory syndrome (MERS) coronavirus and SARS-CoV-2.7
Emerging evidence, though limited, has shown venous thromboembolism as a complication of COVID-19.8 The possible mechanism may be that coronavirus attacks the human body through the enzyme ACE2, which is distributed over blood vessels and various organs.9 The virus then causes cytokine storm, which can increase blood clotting problems and damage. Finally, the blood clots of deep vein thrombosis can be caused by anything that prevents blood from circulating or clotting normally, such as injury to a vein, surgery, certain medications and limited movement but the exact cause of deep vein thrombosis caused by COVID-19 is still unknown.
Viral infections can cause an imbalance between pro- and anticoagulant states during the course of the disease and it is often associated with the disruption of the vascular endothelium.10 Several pathways involving the coagulation cascade, including raised von Willebrand factor, can lead to the development of fibrin clots. These clots breakdown, resulting in the elevation of D-dimer levels and fibrin degradation product levels. Both of these are tied to poor prognosis in COVID-19 patients, including the need for ICU admission, and death. The activation of systemic coagulation, associated with the immobility due to bed rest heightens the risk of venous thromboembolism.
Klok et al and Middeldorp et al8,11 advise against prophylactic treatment-dose anticoagulation in patients with COVID-19 admitted to the hospital and advocate the use of a lower threshold for diagnostic tests to assess thrombotic complications including deep vein thrombosis and pulmonary embolism. More research is required to understand if pre-emptive and prolonged treatment dose anticoagulation results in a favorable clinical outcome in patients with COVID-19 infection.
CONCLUSION
As COVID-19 continues to lead to significant mortality, more data is emerging that is exposing its perplexing pathogenicity. Meanwhile, the presentation of venous thromboembolism in patients with COVID-19 remains an unusual finding. It is imperative for healthcare providers to be mindful of this unique association to make necessary diagnostic evaluations and provide appropriate treatment for the patients.
REFERENCES
- Centers for Disease Control and Prevention. https://www.cdc.gov/flu/symptoms/flu-vs-covid19.htm
- World Health Organization. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19
- World Health Organization. Coronavirus disease (COVID- 19) pandemic. Situation reports. Available at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---18-may-2021
- Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259-60.
- Clinical Management Protocol: COVID-19. Available at: https://www.mohfw.gov.in/pdf/ClinicalManagementpdf
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al; China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-33.
- (1 May 2020). Retrieved from: https://www.niaid.nih.gov/diseases-conditions/coronaviruses. Accessed May 6, 2020.
- Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-7.
- Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586-90.
- Atallah B, Mallah SI, AlMahmeed W. Anticoagulation in COVID-19. Eur Heart J Cardiovasc Pharmacother. 2020;6(4):260-1.
- Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Müller MCA, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18(8):1995-2002.